Ready to optimize your revenue cycle?
At AlignMed RCM Services, we streamline your medical billing process, ensuring accurate claims submission, faster reimbursements, and maximized revenue. Our expert team handles everything from charge entry to payment posting, reducing denials and optimizing your financial performance.

✅ Accurate Claims Processing – Minimize errors and improve first-pass acceptance rates.
✅ Experienced Billing Specialists – Professionals handling complex billing procedures.
✅ Fast & Efficient Reimbursement – Get paid faster with optimized RCM.
✅ Comprehensive Compliance – Stay up-to-date with regulations and avoid penalties.
✅ Customized Solutions – Tailored services to fit your practice’s unique needs.
✅ 24/7 Support – Dedicated assistance whenever you need it.
Approach and Benefit.
We take a patient-centered, provider-focused approach to billing, ensuring smooth operations and financial growth.
We offer affordable pricing packages tailored to practices of all sizes, helping you save costs while improving cash flow.
We ensure full compliance with HIPAA and other industry regulations, keeping your data safe and confidential.
With our proactive denial management strategies, we significantly reduce claim denials and maximize reimbursement.
Why Medical Billing is Crucial for Healthcare Providers?
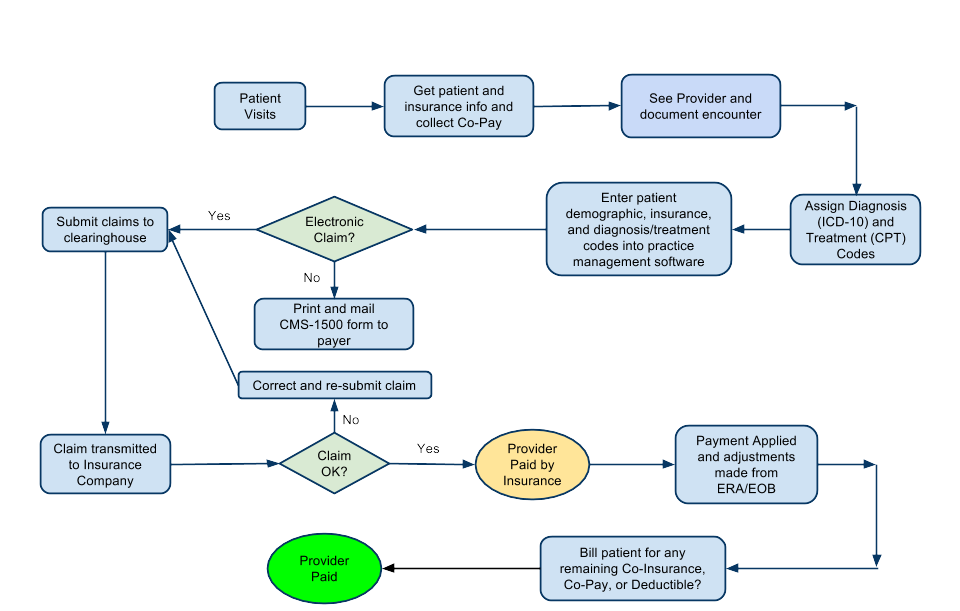
Medical billing is the heart of a practice’s financial health. It ensures that healthcare providers receive timely and accurate reimbursements for services rendered. A well-managed medical billing system minimizes claim denials, reduces payment delays, and increases overall revenue.
At AlignMed RCM Services, we specialize in end-to-end medical billing solutions, allowing physicians, clinics, and hospitals to focus on patient care while we handle the revenue cycle.
